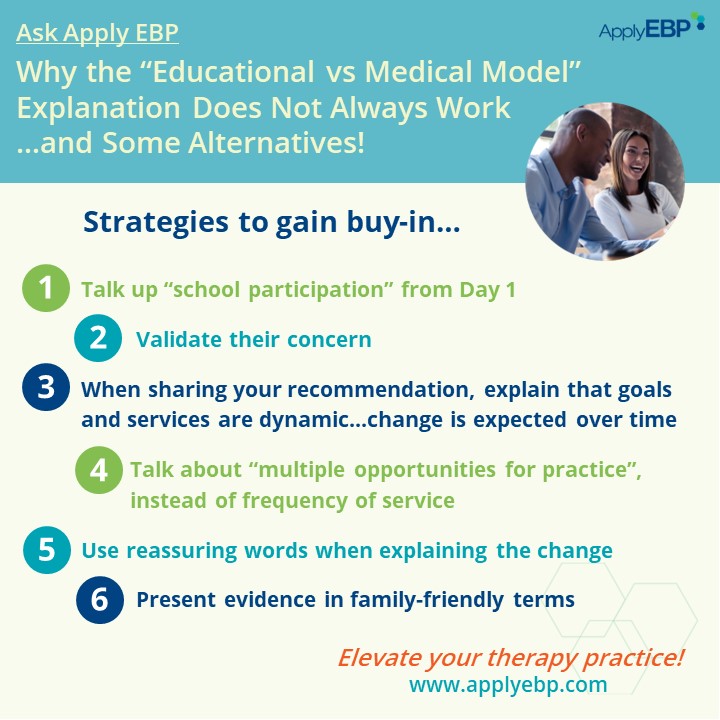
Ask Apply EBP
What to Do When the “Educational vs Medical Model” Explanation Does Not Work
Q: I need help to get buy-in from the team about a change in services, and discussing educational versus medical does not seem to be working. Any suggestions?
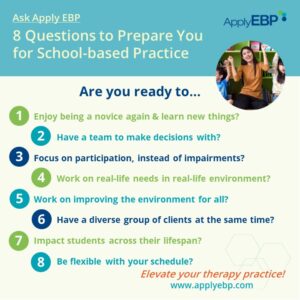
A: Such a great question that shows not just your concern as a school-based practitioner, but also reflects the concern of the family and the team. There are times when talking about educational versus medical models may be a great way to explain your role in the school, such as when you are doing an in-service for your school team, or when you are answering the question “OT? I did not know OTs work in schools. What do you do in school?”
However, as you may have found out already, the educational versus medical models may not always be the best way to explain your service recommendation, especially when you are suggesting a change in services. Why?
3 Reasons Why Educational and Medical Models Conversation May Not Work
-
-
- To families and educators, it may sound like we are not willing to help the child.
- While this is not what we mean, if we put ourselves in their shoes, we have to admit that the educational versus medical model explanation can sound like “This is not my problem!”
- At times, we have referred children to, say, outpatient services, in cases where we know a medical model would not help the child with a particular goal either.
- Instead of having an honest conversation with the family and educators, we have sometimes passed the “problem” on to somebody else.
- Yes, therapists in clinics have done the same to school-based practitioners. They have referred children for school-based services that are not appropriate.
- But we have also done the same to them. We have referred when we know or suspect based on our knowledge of the student’s condition and of the effectiveness of interventions, that there is nothing they can offer either to help the child reach an inappropriate goal.
- When the family and the team have heard the educational versus medical model conversation many times and we still can’t get buy-in, it just means it’s time to move on and explain ourselves in a way that may relate better to their expressed concerns.
- To families and educators, it may sound like we are not willing to help the child.
-
So what might be some better ways? Read on…
6 Strategies for Getting Buy-in on a Change in Service
Getting buy-in requires understanding of our roles and trust that we are there for the student. This takes time! So we provide you with strategies you can utilize when presenting your recommendation for a change in service, and other strategies that you should employ from the first day you meet with families and/or educators so you can get them on your side when the time comes for you to make a recommendation.
Strategy #1: Talk up “school participation” from Day 1
To make sure that the family differentiates you from medical-based practitioners, talk up school participation from Day 1. That is what makes you different from medical-based practitioners.
Review your assessment, goals, and interventions. How much do they cover body function and structure, and impairments? How much do they cover participation? If you see more references to body function and structure than participation, then that may be the reason why families and educators confuse you with medical model providers.
Here are some changes you can do so your role as a school-based therapist becomes clearer:
-
-
- Start your assessment at the participation level! And when you write your report and present it at a meeting, highlight the student’s level of participation in various areas of the schools. Yes, use the word “participate” or “participation” as much as you can, or whatever variants thereof, such as “play with their peers”, “complete their classwork”, “eat meals with their classmates”, etc.
- Create goals with the team that focuses on the student’s participation in meaningful occupations.
- Try to avoid anything that implies “fixing” their child. Find and celebrate their strengths, and use these strengths to help them accomplish their goal.
- When explaining your role, we challenge you to not use the phrase “educational versus medical” and see if you can deliver the same message to demonstrate to the family and educators your concern for the student’s success in school.
- For example, you can say
- “There are definitely overlaps in what [OTs/PTs/etc.] do in schools and outpatient settings. As a school-based [OT/PT/etc. provider], my service is provided when the student [or your child] needs it to achieve their IEP goals.”
- “As a related service provider, I am here to support the educational team in maximizing your child’s participation in school.”
-
Strategy #2: Validate their concern
This is a golden strategy that I learned from Peggy Morris. It goes a long way in demonstrating to the family and educators that you are there for their child/student and that everything you are doing and saying is in line with their concern.
-
-
- There will be time to talk about solutions later. When you validate, you are simply affirming that you hear them.
- Ask them about their concern and goals for their child. Show acknowledgment by repeating their concern and goals.
- This validation has another function for your own clinical reasoning. By repeating their concerns and goals, you are also making sure that you heard them correctly.
-
Strategy #3: When sharing your recommendations, explain that goals and services are dynamic…change is expected over time
Your current recommendation is based on the current information you have. Doctors do this all the time when they explain the benefits and expected outcomes of an intervention…we should do the same!
I have yet to hear a doctor say, if we do this, you will be cured 100%! And like doctors, we should explain early on that should something not work, what other options can we try? Present various options early to help the child reach their goal.
For example, handwriting is amazing, but typing can work just as well in expressing our thoughts, especially if we have to write a long paper. (That’s how I’m writing this article by the way. I love how easy it is to delete, edit, etc. And the spell-check and grammar-check – priceless!)
Explain that as you work with the student, you gain more information that may result in a change in your recommendation. Make sure you gather data as you provide interventions so you can support your recommendations for changes in goals and services later on.
For a deeper discussion on data gathering to support recommendations, read the article 3 Reasons to Discontinue Pediatric/School-based OT, PT or Speech Services
Strategy #4: Talk about “multiple opportunities for practice”, instead of frequency of service
Frequency of service is a FALSE explanation. For families and educators, it implies that the student would only improve the more we see them. No wonder they have a hard time with a decrease in services!
Explaining that our role is to create “multiple opportunities for practice” for their child makes it less about us, and more about their child. This can apply to any skill they need to practice, from motor skills, to communication, displaying productive behaviors, building friendships, performing self-care, etc.
Discuss how your services are giving their child multiple opportunities to practice a skill they need to master throughout their day even when you are not around. Some examples:
-
-
-
- Who has been coached to support the child’s multiple opportunities for practice?
- How has the physical and social environment been modified to be more supportive of success when they practice the skills?
- How often is practice occurring? With this last one, it would be better if you can show a chart of the child’s day adding up the total minutes of practice. This would show how much more time they get to practice the skill, compared to just working on the skill in a therapy session for, say, 30 minutes a week.
-
-
Strategy #5: Use reassuring words when explaining the change
Be aware that parents may experience grief or a sense of “giving up” when they are told the first time that their child needs assistive technology to perform a task. In the same way, a reduction or the discontinuation of services can be seen as a loss of needed support for their child.
Here are some examples of reassuring terms:
-
-
-
- Using an assistive technology “in parallel”
- For example, writing for shorter tasks, and typing for essays so their child can focus on sharing the amazing thoughts they have quickly and effectively
- Or using a wheelchair for longer distances so their child gets to the playground with lots of energy reserved for playing with their peers using their walker
- “I would like to pilot…”
- Another Peggy Morris classic!
- This implies you are trying something and you will be there to monitor it to make sure it works
- Celebratory words or phrases like,
- “Graduation” instead of discharge or termination of services
- “Johnny has done amazing in [describe improvement here]…with my support. Now he is ready to be given the opportunity to practice as independently as possible.”
- Highlight the student’s strengths. Make a big deal of the achievement, because it is a big accomplishment!
- Using an assistive technology “in parallel”
-
-
Reassure them that related service is not one-and-done. You will be in the school and re-assess their child as needed .
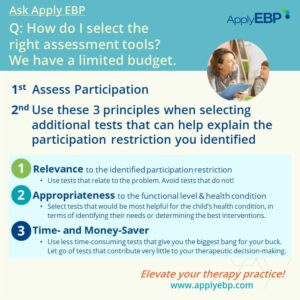
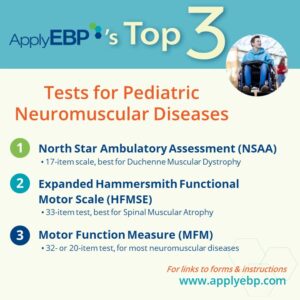
Strategy #6: Present evidence in family-friendly terms
Families and educators would like to hear what works! This builds confidence and trust as it shows that we are science practitioners, and that there is evidence and reasoning to what we recommend! Not just us saying so.
Where appropriate, share something that supports your recommendation. Avoid being jargony. Share studies that relate directly to their concerns and goals.
-
-
- “I know you would like Johnny to get better at…I have learned from this latest research that he can achieve it by…”
- “I attended this seminar last month, where the speaker cited this research that to improve [insert goal here] we need to do…”
-
Present evidence on creating “multiple opportunities for practice” via the approaches below. Share the evidence that indirect services can be just as effective as direct services.
-
-
- Embedded services
- Coaching
- Collaborative consultation
- Context-focused interventions
- Contributions of practice at home – lots of research in this area; this may be a good place to start to find those research
-
Combine these Strategies!
These suggestions are not silver bullets. When you use this new messaging, know that it may be the first time the family, educator, and/or school administrator are hearing the message presented this way. What you are saying may clash with what they may have heard in the past. So often, it takes a consistent use over time of a combination of these strategies before we get buy-in. And I would argue that doing these are worth the investment for building trust and establishing your expertise with the team!
I’m sure there are other great suggestions from all of you. Add them to the comments down there!
If you want to learn more about this topic, join…
Find More Answers to Your Questions in Our...
Featured School
Symposium
6th Online School-based OT and PT Symposium - On-demand Version
- Watch and re-watch on your own time
- On-Demand Version
- OTs, OTAs, PTs and PTAs
- $399-449
Featured Live
Workshop
Deciding Need & Amount of School-based OT/PT
- November 19, 2024, 8:30 am - 3:30 pm Eastern Time
- Online via Zoom
- OTs, OTAs, PTs and PTAs
- $199-249
Featured On-Demand
Webinar
Assessing School Participation
Featured Webinar
Bundle
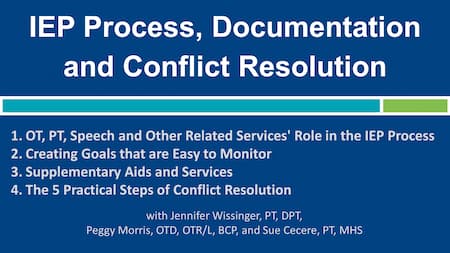
The IEP Process, Documentation & Conflict Resolution Bundle
Have a question?
Submit here…
*Clicking submit will send your question directly to our email inbox. Your name and email will let us know that your submission is real (not spam). We will not include these in our posts, unless you tell us to include your name. Please read our privacy policy here.
All infographics and videos on www.applyebp.com are intellectual properties of Apply EBP, LLC
You may use the infographics and videos for free for any non-commercial, educational purposes. Please cite the source as “Apply EBP, LLC” and a link to the source article. If you plan to use any infographic or video for commercial purposes (i.e., for profit), please email Carlo@applyebp.com to obtain a written permission. Permission can be granted on a case-by-case basis.